Several weeks ago, Derek Malone sat outside Cook County’s Fantus Clinicin the brilliant fall sunshine, looking tired and discouraged.

His stomach hurt and he felt dizzy. It’d been weeks since the 55-year-old had taken medications for his high blood pressure and intestinal ailments – prescriptions he says he can’t afford.
“Ten dollars for a co-pay, I don’t have that,” said Malone, who’s been unemployed and homeless since earlier this year, when his daughter lost a job at a McDonald’s and stopped paying her father to look after her four young children.
“I have zero income, and I get no kind of benefits,” Malone said as resignation crept into his gravelly voice. “The future, man it’s bleak for poor folks like me. I ain’t got no cell phone, no medical card, nothing. You can’t sleep in the streets, the police run you out of the parks. These programs out there, to them I ain’t nothing but a number. It’s a mighty hard pill to swallow.”
Malone has no idea that people in his situation – impoverished adults without dependent children – will be offered assistance starting in 2014 under national health reform, should that legislation survive political and legal challenges.
This lack of awareness isn’t an anomaly: in over a dozen interviews on Chicago’s South and West sides, needy men and women admitted they had never heard of health reform and had no understanding of what it might mean to them.
Told by a reporter that poor adults will benefit from the government’s reform plan, some of these Chicago residents expressed surprise and satisfaction, while others voiced mistrust and skepticism.
“It sounds good,” said Theodora Bell, 56, a South Sider with diabetes, high blood pressure and a bad heart who got a Medicaid card a year ago after qualifying for Social Security disability benefits. “Everybody needs insurance because a lot of times, if you don’t have it, doctors don’t even want to see you.”
But after a moment’s reflection, Bell hedged her enthusiasm. “Let’s see what happens with it,” she said, cautiously. “Let’s see if them’s that needs help really gets it.”
This gaping chasm between policymakers deciding how to implement health reform, politicians debating the value of this groundbreaking legislation, and residents of some of Chicago’s poorest neighborhoods – many of whom appear to have no idea how reform might impact them – highlights a critical challenge for the groundbreaking initiative that’s come to be known as Obamacare.
“How do we get the word out and educate people? That’s discussed at every meeting I attend,” said Dr. Javette Orgain, chairman of the Illinois State Board of Health and associate clinical professor of family medicine at the University of Illinois at Chicago Medical Center. Her answer: “We’ll have to reach people where they get services and enlist every part of the community – churches, public aid offices, Social Security offices, social service agencies, rehab programs, clinics, all of them have a role to play.”
The basic ingredients of health reform that need to be communicated have far-reaching significance for South Siders and West Siders, as they do for people across Illinois:
For the first time, all adults who earn up to 133 percent of the federal poverty level will qualify for Medicaid, the government’s health program for the poor. (In 2011, that threshold represented a yearly income of over $14,400 for a single person and over $29,700 for a family of four.) In Illinois, adults without dependent children haven’t previously qualified for Medicaid even if they were destitute.
State officials estimate that 500,000 to 800,000 people will be added to the Medicaid rolls in Illinois in 2014, when this provision goes into effect. Most will be single adults or married couples without children.
The Medicaid expansion is certain to affect tens of thousands of people on the South and West sides, where poverty and a lack of health insurance are widespread.
Who will care for new Medicaid members is an open question. Because of budgetary pressures, community-based clinics haven’t yet received funds for a major expansion, as originally contemplated under health reform.
“I think there is the potential for a perfect storm” over access to care if health centers aren’t able to expand to meet impending needs, said Dr. Lee Francis, president of Erie Family Health Center, which serves over 34,000 needy patients a year at 11 sites in Chicago.
Dr. Arthur Jones, a health care consultant and chief medical officer for Medical Home Network, a new healthcare initiative on the Southwest side, said he worried that “there really may not be enough primary and specialty care physicians to deal with this population.”
Indeed, a June 2011 study in the New England Journal of Medicine found that specialty clinics across Cook County denied medical appointments to 66 percent of people posing as Medicaid members seeking care for sick children. If financial pressures on Medicaid escalate as health reform proceeds – a likely scenario – difficulties with accessing care might become even more acute.
Judith Graham has covered health policy for dozens of years. For many years, she was a health and medicine correspondent at the Chicago Tribune. Her work has appeared in the Washington Post, Los Angeles Times, Baltimore Sun, Philadelphia Inquirer, Seattle Times and the New York Times, among other publications.
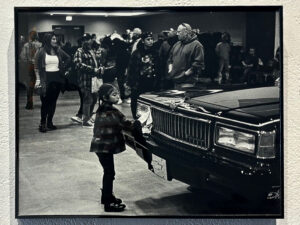
For our “Waiting for Health Care Reform” video, click here – for a slideshow, click here. For all our health-care videos in HD, visit IHM’s new Vimeo channel.










Be First to Comment